Marissa O. Coppin
Architecture in Drosophila Mutants
Abstract:
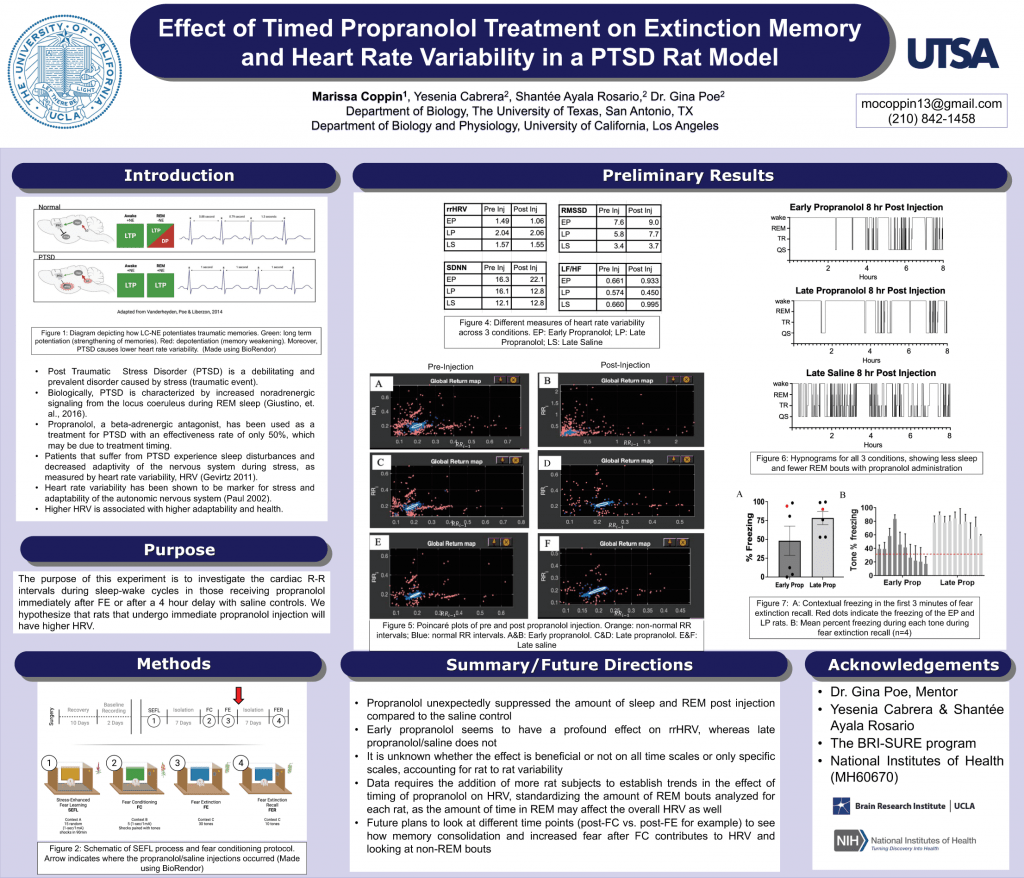
According to the American Psychiatric Association, 1 in 11 people will develop Post Traumatic Stress Disorder (PTSD) in their lifetime. Patients that suffer from PTSD experience many symptoms, including sleep disturbances and decreased adaptivity of the nervous system during stress, as measured by heart rate variability (HRV). Biologically, PTSD is characterized by an increase in signaling of noradrenaline from the locus coeruleus during REM sleep, which is more activated post-trauma. Since depotentiation, the weakening of the synapses of memories, can only occur during REM sleep in the absence of noradrenergic signaling, those with PTSD retain the full weight of emotions in their traumatic memories. Propranolol, a beta-adrenergic antagonist, has been used as a treatment for PTSD with an effectiveness rate of only 50%. We hypothesize that consideration of the timing of propranolol administration in relation to sleep will make the difference between effective and ineffective treatments. Administering propranolol after fear extinction (FE) learning but before REM sleep would show reduced freezing during FE recall, as extinction learning requires weakening of old fear memory associations. In addition, we expect propranolol-treated rats to show increased HRV, reflecting better adaptability. Therefore, we propose to investigate the cardiac R-R intervals during sleep-wake cycles in those receiving propranolol immediately after FE or after a 4 hour delay with saline controls. We hypothesize that rats that undergo immediate propranolol injection will have higher HRV. This study would provide increased understanding of post-stress autonomic system regulation and insight into effective ways to reverse the symptoms of PTSD.